Abstract
Background
Adolescents and young adults (AYAs) with sickle cell disease (SCD) are at increased risk for disease complications and mortality, particularly during transition to adult care. Little is known about the disease course that might be contributing to the increase in morbidity and mortality during transition. This study provides a longitudinal description of the clinical characteristics and disease severity among AYAs with SCD during transition to adult care.
Methods
We conducted a longitudinal analysis of the electronic health records of 339 AYAs (ages 12-27 years) with SCD (97% black, 56% male, 69% hemoglobin SS) who received care at a comprehensive SCD center in the Southeast US between 1989 and 2015. Measures included sociodemographics, transfer, complications, comorbidities, and severity of SCD (using a modification of the pediatric SCD severity index).
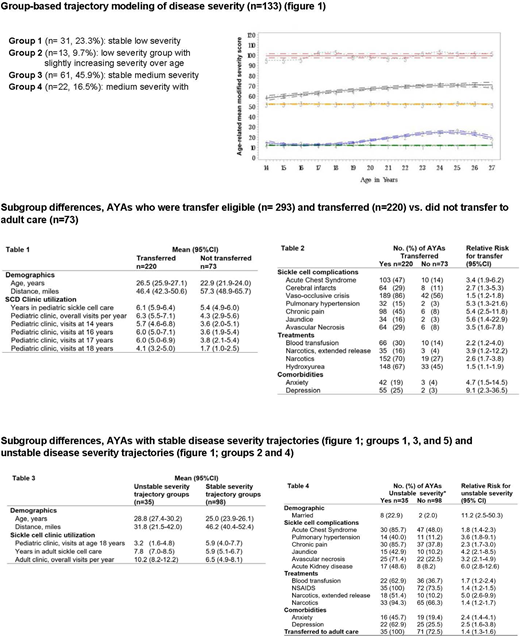
We used group-based trajectory modeling to identify subgroups of AYAs with distinct severity trajectories. AYAs who were in care for at least 10 years were included (n=133). We used chi-square and unpaired student t-test to explore subgroup differences among (1) AYAs who died compared to AYAs who were still alive during the study; (2) AYAs who were eligible to transfer (i.e., ≥ 19 years) (n=293) and transferred compared to AYAs who were eligible to transfer and did not transfer; and (3) AYAs with different severity trajectories. Statistical significance was set at p=0.05 and 95% CI.
Results
Common complications among AYAs (n=339) included vaso-occlusive crises (80%), acute chest syndrome (41%), chronic pain (35%), and cerebral infarcts (22%). Comorbidities included depression (19%) and anxiety (14%). Most AYAs who were eligible to transfer transferred (n=220, 75%) at a mean age of 19 years (SD=1.3). Fourteen AYAs died, 10 (71%) after transfer at a mean of 7.3 years (SD=3.1) from transfer.
SCD Severity Trajectories (Figure 1): Group-based trajectory modeling identified both stable and increasing severity trajectory groups: stable-low (n=31, 23%), stable-medium (n= 61, 46%), stable-high (n=6, 5%), low-increasing (n=13, 10%), and medium-increasing (n= 22,17%) severity trajectory groups. Most AYAs (74%) had stable severity over time, whereas 26% had increased severity with increasing age.
Subgroup Differences in Care and Mortality: AYAs who died (n=14) spent less time in pediatric care (mean=4.6 years, 95%CI 3.7-5.6), however, had a higher mean number of pediatric annual visits (mean=9.3 visits; 95%CI 6.3-12.3) compared to those who were alive (n=324, mean=6 years in pediatric care, 95%CI 5.7-6.1; mean number of pediatric annual visits=5.4, 95%CI 4.8-6.1). There were no differences in demographics, SCD complications, or morbidity.
Subgroup Differences in Transfer to Adult Care (Tables 1 and 2): Compared to AYAs who did not transfer, AYAs who transferred were older and lived closer to the SCD clinic. AYAs who transferred were at higher risk for SCD complications and comorbidities. They were more likely to be receiving hydroxyurea. They had higher mean annual pediatric SCD clinic visits, especially during older adolescence, and were in pediatric care for a longer duration.
Subgroup Differences in Disease Severity (Tables 3 and 4). Compared to AYAs in stable severity trajectory groups (Figure 1: Groups 1, 3, and 5), AYAs in unstable disease severity trajectory groups (Figure 1: Groups 2 and 4) were more likely to be married, older, and lived closer to the SCD clinic. AYAs in unstable groups were also at higher risk for SCD complications and comorbidities. They were less likely to be receiving treatments and had less pediatric SCD clinic visits by age 18. However, they were more likely to transfer to adult care, have had more adult SCD visits overall, and remained longer in adult SCD care after transfer.
Conclusions
Whereas most AYAs with SCD had stable disease severity, nearly a quarter had increasing disease severity, over time. AYAs with increasing severity lived closer to the SCD clinic, were more likely to transfer to adult care, and demonstrated higher and longer use of adult SCD care compared to AYAs with stable disease severity. Genotype was not associated with disease severity trajectory groups, underscoring the importance of clinical care for AYAs, over time.
Kayle:Department of Health and Human Services, Administration for Community Living, NIDILRR Advanced Rehabilitation Research Training Health and Function Grant #90AR5019 (PI Heinemann): Other: post-doctoral fellowship; Department of Health and Human Services, Administration for Community Living, NIDILRR Advanced Rehabilitation Research Training Health and Function Grant # 90ARHF0003 (PI Heinemann): Other: Postdoctoral fellowship. Tanabe:Duke University: Employment; NIH and AHRQ: Research Funding; Alliant Health: Consultancy. Maslow:The Crohn's and Colitis Foundation and the American Gastroenterological Association, in collaboration with Pfizer, Inc: Research Funding. Holl:Before Brands, Inc: Research Funding; NIH: Research Funding; Branstad Family Foundation: Research Funding; AHRQ: Research Funding. Shah:Novartis: Research Funding, Speakers Bureau.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal